- Conditions
- Foot drop
Foot drop Paresis of the tibialis anterior muscle / paralysis of the tibialis anterior muscle
Introduction
Foot drop is a condition in which the foot can no longer be placed on the ground in a controlled manner when walking. The foot flops down, so to speak, once the heel has made contact with the ground. Or the foot can no longer be raised at all and "drags" on the ground. There is no longer any control, because the muscles in the lower leg are weakened or have failed completely due to a problem with the nerve.
Foot drop is also called paresis of the tibialis anterior muscle or paralysis of the tibialis anterior muscle.
Description of condition
Foot drop is characterized by the loss of function of the muscles that raise the foot, known as the tibialis anterior muscles. Because the tibialis anterior muscles have weakened, they can no longer control the placement of the foot. Or the foot can no longer be lifted in its entirety so that the foot drags on the ground.
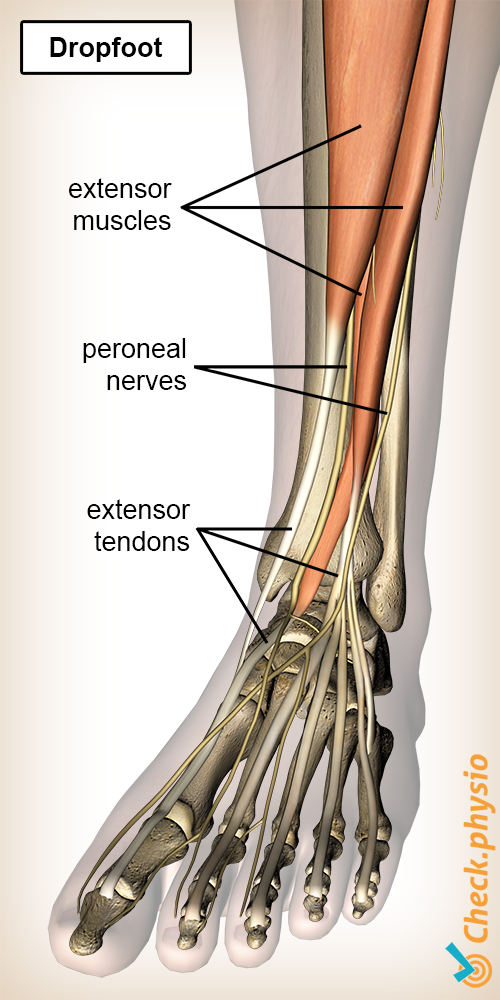
The muscles responsible for lifting the foot are:
- Tibialis anterior muscle.
- Extensor hallucis longus muscle.
- Extensor digitorum longus muscle.
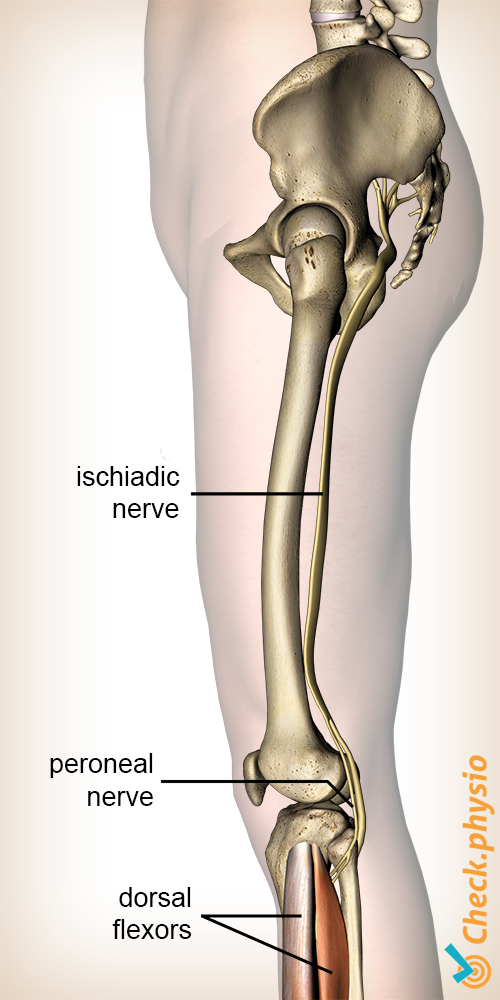
These muscles are controlled by the same nerve, the common peroneal nerve. When damage or pinching occurs somewhere along the length of the nerve, there is a chance that the muscles will no longer work properly.
Nerves originate in the spinal cord. The common peroneal nerve branches from the large leg nerve. This one is composed of nerves originating from the lower five vertebrae. The large leg nerve runs along the back of the hip, via the rear of the knee, toward the lower leg. The common peroneal nerve splits into two smaller branches in the lower leg.
Cause and history
Pressure on the peroneal nerve can develop as a result of acute trauma, but a more gradual onset can also occur. Trauma may occur if the nerve is suddenly subjected to a major traction force, compression force or sudden shift, such as an hernia . This causes foot drop due to pressure on the nerve in the spine.
Signs & symptoms
A trapped nerve usually follows a fixed pattern with clear characteristics of a loss of motor (muscle) and sensory (sensation) functions.
With foot drop, the main symptoms are:
- Inability to lift the front of the foot.
- No control or reduced strength of the muscles in the lower leg.
- Impaired gait.
These are the symptoms that are immediately noticeable. In addition, there are other symptoms that can be traced back to the point where the nerve is pinched:
- Muscle weakness in the hip muscles.
- Muscle weakness in knee flexors.
- Muscle weakness in tibialis anterior muscles.
- Muscle weakness in toe extensors.
- Inability to walk on the heels.
In addition, sensory disorders may be present when touching the skin. Or all feeling is completely absent in certain places on the leg:
- Lateral side of the thigh.
- Side of the lower leg.
- On top of the foot.
- Inside of the foot.
- Between the first and second toe.
Diagnosis
The diagnosis of foot drop is usually easy to make, considering the change in gait pattern and the reduced strength of the tibialis anterior muscles. Finding the cause of foot drop is more difficult. This is due to the large overlap of symptoms in the innervation area.
In order to gain a clear insight into the problem, it is very important to ask the patient some questions. Symptoms such as back pain, any possible cause and the course of the symptoms are important for a correct diagnosis.
Afterwards, a physical examination needs to be carried out. This is to find out which muscles are weakened and where sensory changes have occurred. Reflexes also need to be tested in case foot drop is suspected due to a cause originating in the spinal column.
When in doubt, or for verification purposes, the location of the entrapment can be examined with an EMG (nerve conduction test). If compression is suspected to be caused by a bone disorder or if it originates in the back, an MRI may be required to confirm this.
Treatment and recovery
The treatment is often conservative, i.e. without surgery. Only if there is compression due to bone disorders or other structural impingements, will surgery be a solution. This removes the compression.
The physiotherapist often assists patients who have these symptoms, although it is not usually necessary to see the physiotherapist frequently. Progress can be monitored well using targeted exercises and by regularly checking muscle strength. Foot drop can often show a recovery within a few months, but recovery can also take a year. If the physiotherapist does not see any progress in this period, or if it gets worse, further examination will be necessary. Besides physiotherapy, other possibilities include custom-made soles or a brace.
The treatment of foot drop that originates from the spine consists primarily of treating the spine.
Exercises
Take a look at the online exercise program with exercises for the drop foot.
More info
You can check your symptoms using the online physiotherapy check or make an appointment with a physiotherapy practice in your locality.
References
Haveman, J.W. & Blomme, A.M. (2009) Beknelling van de N. peroneus superficialis. Een karakteristiek klachtenpatroon Ned. Tijdschr. Geneesk. 2009;153:B268; Isala klinieken, afd. Chirurgie, Zwolle.
Magee, D.J., Zachazewski, J.E., Quillen, W.S., Manske, R.C. (2016) Pathology and intervention in musculoskeletal rehabilitation Elsevier, 2nd edition.
Krishnamurthy, S. & Ibrahim, M. (2019) Tendon Transfers in Foot Drop Indian J Plast Surg. 2019 Jan; 52(1): 100–108.